Motherhood is seen as an unforgettable, blissful, and miraculous experience, which is true. However, there is a dark side to it that we rarely address.
The emotional, physical, and psychological torture that mothers experience throughout the pregnancy journey remains hidden. It is often regarded as a woman-only secret or taboo. In this era of knowledge, we cannot overlook the side effects of pregnancy.

In this article, let us look at the less-talked-about side effects associated with pregnancy and childbirth. So many questions are running through your head right now: Why do some people frown upon pregnancy? Which side effects are associated with pregnancy and childbirth? When should you seek medical help for pregnancy-related side effects?
Why do People Talk Less About Pregnancy-Related Effects?
In the last article on pregnancy symptoms, we tackled more than 5 common symptoms. However, we failed to address the side effects that come with such symptoms, including postpartum. There are three reasons why the side effects associated with pregnancy and childbirth fail to see the light of day:
i. Societal Pressure
The society has been conditioned to treat pregnancy and childbirth with so much disgust. Throughout my interaction with more than 50 mothers, I learnt that they were neglected during pregnancy.
One mother admitted, “My husband never got close to me throughout my two last trimesters. He would complain that I snored when asleep and I kept whining of backache. My mother-in-law was also on my neck to do basic domestic chores.”
I sighed. I empathized with the lady, letting her know that each woman reacts differently to pregnancy.
ii. Lack of Awareness
The second reason why pregnant women or new mothers fail to talk about pregnancy and related effects is due to a lack of awareness. Like I keep mentioning, every woman has a unique pregnancy experience.

The misleading information from “pregnancy coaches” makes mothers and mothers-to-be, leaves more women confused when they experience different symptoms.
In other cases, obstetricians might leave out crucial details on pregnancy and childbirth, bringing in more confusion.
iii. Fear of Being Judged
The mother, whose husband and mother-in-law bullied experienced some form of fear of judgement. She wanted to prove to her husband that she was not an overly pampered big girl. In such cases, women will fear addressing their insecurities and effects, and instead, act as if everything is okay.
Which Physical Effects are Linked to Pregnancy and Postpartum?
As an expectant or new mother, you are likely to experience one or several of these physical effects:
A. Hot Flashes
Hot flashes are a common occurrence in many postpartum women. The most common causes of postpartum hot flashes are:
- Declining estrogen levels- the drop in estrogen might leave the body disoriented, resulting in hot flashes.
- Increase in prolactin (milk-making hormone)- As prolactin suppresses estrogen, it causes hot flashes.
- Increase in cortisol and adrenaline levels- The two hormones are linked to postpartum exhaustion, insomnia, and hot flashes.
- Postpartum thyroiditis imbalance, which affects 5-10% of new mothers, might cause hot flashes.
Postpartum Hot Flashes Symptoms

These are the most common symptoms of postpartum hot flashes.
- Sudden heat surges (face, neck, chest)
- 💦 Drenching sweats, especially at night
- ❄️ Chills afterward (from rapid cooling)
- 😰 Anxiety or heart palpitations during episodes
- 🕒 Triggers: Warm rooms, caffeine, spicy foods
How to Manage Postpartum Hot Flashes
These are the most effective ways of managing postpartum hot flashes.
- Dress well- When the hot flashes come knocking, take off some clothes or turn on the fan.
- Cool down your area of sleep- Sleeping with a damp cloth or chill pillow would be effective.
- Hydrate- Keep sipping your fluids to remain hydrated all through. While at it, avoid alcoholic or caffeinated drinks.
- Balance your blood sugar- Prioritize protein and fiber-rich foods with low carb and sugar levels.
- Avoid stress- Try postpartum meditation, go for therapy, and avoid any stress-causing issues.
When to See a Doctor for Hot Flashes
These are incidents when you should see a doctor to help you handle hot flashes. These include when:
- They last beyond 6 months
- They are accompanied by dizziness, rapid weight loss, or irregular heartbeat
- They disrupt daily life or mental health
B. Hemorrhoids and Anal Fissures
I tackled the issue of hemorrhoids and anal fissures in this article. Kindly go through it and understand why postpartum mothers shy away from addressing the pain they undergo due to it.
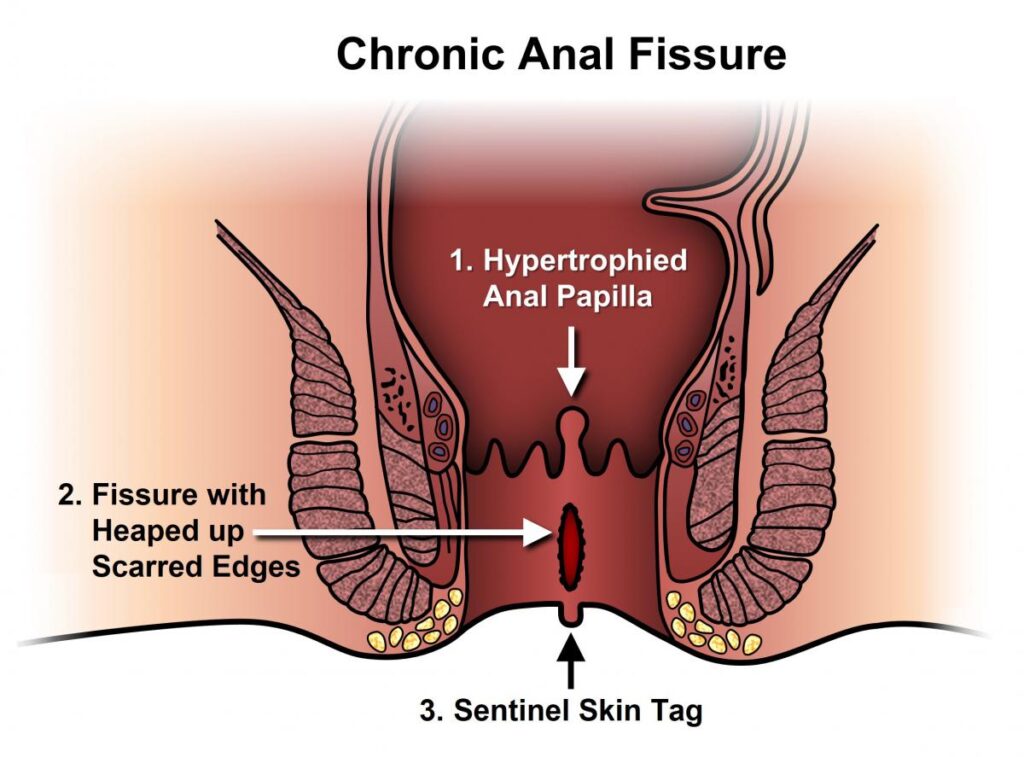
As a new mother, you should not shy away from talking about the challenges that come with hemorrhoids and anal fissures.
You can suppress the pain and discomfort of hemorrhoids and anal fissures by following these tips:
- Using witch hazel pads
- Taking warm sitz baths
- Eating high-fiber foods to avoid constipation
C. Postpartum Hair Loss
Healthy hair means so much to many women, and losing it during pregnancy or after delivery leaves them devastated. Some women might experience thinning hair or excessive shedding, while others experience changes in texture. Regardless of the hair loss intensity, the experience makes women lose esteem.
Causes of pregnancy and postpartum hair loss
There are several causes of pregnancy and postpartum hair loss:
- Hormonal changes- A Drop in estrogen levels after delivery causes the hair to go into the telogen phase (hair shedding).
- Postpartum Thyroid Issues- About 5-10% of postpartum mothers lose hair due to a drop in the hypothyroidism hormone.
- Nutritional Deficiencies- A drop in iron and other nutrients such as biotin, vitamin D, and zinc causes postpartum hair loss.
What are the Symptoms of Postpartum Hair Loss?
In my last article on postpartum hair loss, I focused on babies. Let us now look at the most common symptoms of postpartum hair loss that mothers get:
- Clumps of hair in the shower, brush, or pillow
- 🔹 Widening part or thinning at the temples
- 🔹 Brittle, dry hair (due to nutrient depletion)
- 🔹 Peak shedding at 3-4 months postpartum (can last 6-12 months)
How to Manage Postpartum Hair Loss
These are the most common ways through which you can manage hair loss:
- Be gentle
- Avoid using brushes on wet hair and instead use a wide-tooth comb (as shown below).

- Avoid tight ponytails, braids, or heat styling, which can stress your hair.
- Observe a healthy diet.
- Eat healthy meals such as foods rich in vitamin D, biotin, protein, and iron.
- Avoid sugar-rich or junk foods
- Try Scalp Massages
Massaging your scalp gently helps in:
- Stimulating blood flow to follicles.
- Supporting hair growth.
- Taking Postpartum Supplements
- Prenatal vitamins (continue if breastfeeding).
- Collagen peptides to reduce shedding.
- Avoid Over-Washing
After delivery, the hair becomes delicate and you should avoid over-washing.
- Shampoo 2- 3x/week with a sulfate-free formula.
- Try a volumizing spray for thinning areas.
D. Weakened Pelvic Floor
Childbirth leaves your body disoriented, and your pelvic floor is not exempt from these changes. If not managed early, a weak pelvic floor can leave a mother devastated and with low self-esteem.
Causes of Weakened Pelvic Floor
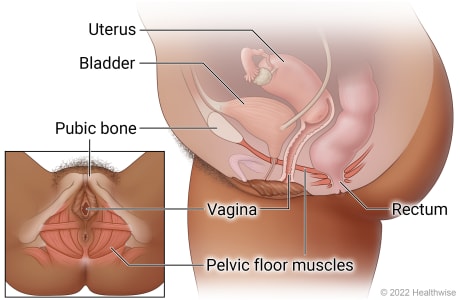
These are the causes of weakened pelvic floor in pregnant or postpartum women:
- Vaginal delivery-The tearing and stretching during delivery weakens the pelvic muscles.
- Pregnancy- The weight of the growing fetus in the womb causes the pelvic muscles to weaken.
- Multiple pregnancies- The more a woman gets pregnant, the more the pelvic floor muscles weaken.
- Large baby and prolonged pushing- Bigger babies (>8.5 lbs) or long labors increase muscle damage.
Symptoms of a Weak Pelvic Floor
- Stress incontinence (leaking when coughing, sneezing, laughing)
- Urgency/frequent urination (sudden strong urges)
- Pelvic pressure or heaviness (feeling like organs are dropping)
- Painful sex (due to muscle tightness or laxity)
- Fecal incontinence or gas leakage (rare but possible)
- Lower back pain (from poor core support)
How to Strengthen Pelvic Floor Muscles
These are the most effective ways to strengthen pelvic floor muscles during pregnancy and after delivery.
Kegel Exercise
Every physical and lifestyle trainer, not forgetting sex “coaches,” recommend kegel exercises. To perform exercise, follow these simple steps:
- Squeeze your pelvic muscles as if you are holding back urine for 3-5 seconds.
- Release the muscles and repeat the process for 3 minutes.
- Repeat the process 5-10 times a day.
Strain Less
- Avoid tasks that strain your body, especially during pregnancy or as a new mother.
- If you cannot access a toilet seat, improvise as demonstrated below, to reduce straining.

Adjust Your Lifestyle
You can adjust your lifestyle to cope accordingly when your pelvic floor muscles weaken by:
- Hydrating frequently to keep your kidneys less intoxicated.
- Keeping your weight at reasonable levels to avoid overwhelming the pelvic floor muscles.
- Limiting strenuous or high-impact exercises such as weight lifting until fully fit.
E. Swollen Feet and Joint Pain
Many mothers fail to mention the mobility issues they face due to swollen feet and joint pain, especially during pregnancy.
The article on pregnancy issues that women face during pregnancy mainly talked about carpal tunnel syndrome.
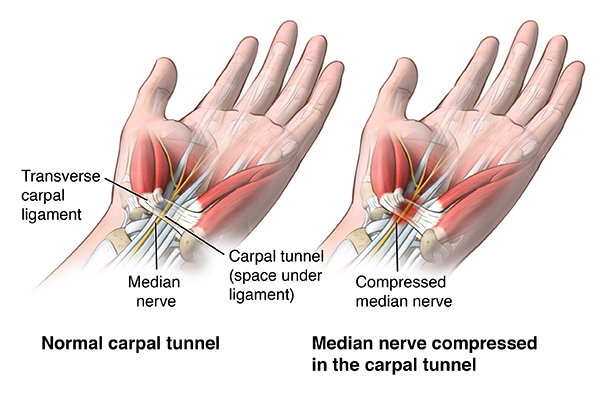
However, the issue of swollen feet is becoming more prevalent during pregnancy, with research showing that 8 out of 10 mothers face the condition.
Causes of Swollen Feet During Pregnancy
Edema or swollen feet during pregnancy can occur due to the following:
- High Blood Volume – The body produces more blood to support the baby, leading to fluid retention, hence the swelling.
- Hormonal Imbalance – Increased progesterone levels during pregnancy cause the blood vessels to relax, slowing down circulation and causing fluid buildup.
- Uterine Pressure – The growing fetus causes the uterus to compress the pelvic veins (especially the inferior vena cava), reducing blood flow from the legs.
- Heat & Prolonged Standing – The weight from the upper body and growing feet causes them to swell.
- Preeclampsia (Serious Cause) – Preeclampsia refers to sudden or severe swelling (especially in hands/face) due to high blood pressure.
Causes of Joint Pain During Pregnancy
Swollen feet during pregnancy are accompanied by joint pain, although this is not always the case. Your joints can be painful due to:
- Relaxin Hormone – The hormone loosens ligaments and joints to prepare for childbirth, leading to instability and pain.
- Weight Gain – Extra weight gain stresses the hips, knees, and lower back joints, causing pain.
- Postural Changes – The shift in the center of gravity strains muscles and joints.
- Fluid Retention – Increased fluid retention may increase pressure on nerves (e.g., carpal tunnel syndrome in wrists).
Management Tips for Swollen Feet:
Here are the best management tips for swollen feet during pregnancy:
- Elevate Your Feet – Keep your feet raised above heart level for 15–20 minutes, 3–4 times daily.
- Hydrate – Drinking water helps flush excess toxic fluids and keeps you fit.
- Wear Compression Socks – Compression socks improve body circulation.
- Avoid Standing/Sitting Too Long – Take short walks to improve blood flow.
- Sleep on Your Left Side – Reduces pressure on the vena cava and improves circulation.
Management Tips for Joint Pain:
These tips will help you manage joint pain easily:
- Avoid High-Impact Exercise – Instead, practice low-impact exercise such as swimming, prenatal yoga, or walking.
- Wear Supportive Shoes – Wear cushioned, low-heeled shoes with good arch support.
- Get Prenatal Massage or Warm Baths – They will relax the muscles and reduce joint discomfort.
- Wear Maternity Support Belt – This belt relieves pelvic and lower back pressure.
- Proper Posture – Avoid slouching; use a pregnancy pillow for sleeping support..
- Pain Relief– Acetaminophen (Tylenol) may be recommended, but under a doctor’s prescription.
F. Loss of Teeth and Loose Teeth
During my interaction with expectant and new mothers, I noticed that some talked or laughed while hiding their mouths. Upon deeper personal interaction, they told me that they had lost their teeth during pregnancy or after delivery.
If your teeth are decaying, aching, or falling off due to pregnancy-related complications, you are not alone. A case study involving 504 women showed that 39% of them experienced similar symptoms.
Weakening or decay of the teeth during pregnancy can be due to the following:
- Hormonal changes
High estrogen and progesterone levels during pregnancy might make the teeth more sensitive, resulting in pregnancy gingivitis.
The relaxin hormone weakens the gums, making the teeth loose and at a high risk of falling off.
- Calcium Redistribution
During pregnancy, the calcium in the mother’s body gets distributed between her and the unborn baby. Thus, if the mother takes food with calcium deficiency, the fetus draws it from her teeth and bones.
Note: If a pregnant woman takes calcium-rich food, the unborn baby does not suck it up from her body.
- Postpartum Neglect
Mothers battling postpartum depression often skip dental care, which results in toothache and decay.
- Dietary Changes
- Some expectant mothers might crave carbs or sugary snacks, which increases the risk of cavities.
- Taking snacks at night with little oral care increases the risk of dental issues.
- Morning Sickness and Acid Erosion
Frequent vomiting due to morning sickness exposes the teeth to stomach acid, erodes the enamel, and causes dental issues.
G. Fistula
Postpartum fistula is a condition that many women speak about in hushed tones. Fistula is treated as taboo and disgusting, with many people staying away from the victims.

Fistula refers to a condition that develops as a result of a tear between the vagina and bladder (vesicovaginal fistula, VVF) or rectum (rectovaginal fistula, RVF). The tear makes it hard for a woman to control her pee or poo, leaving them physically and mentally distressed.
There are several causes of fistula in women postpartum:
Ø Obstructed Labor
Data from the World Health Organization (WHO) shows that between 50,000 and 100,000 women develop fistula each year, with obstructed labor being the major cause.
Obstructed labor occurs when the baby’s head presses the vaginal walls for too long, cutting off blood flow or creating a hole.
- Traumatic Delivery
Mothers can also develop fistula due to traumatic deliveries such as vacuum extractions and unrepaired perineal or vaginal tears.
- Infections and Tissue Damage
Postpartum infections like necrotizing fasciitis can result in fistula when left untreated.
Radiation therapy is also linked with fistula, despite its disassociation with childbirth.
- Surgical Complications
- Rectal or bladder injuries during C-sections can cause fistula.
- Poorly conducted episiotomy can also cause fistula if left untreated.
Pregnancy and Postpartum Emotional and Mental Issues
Pregnancy and postpartum also affect women, leaving them depressed and ashamed of the whole experience. The emotional and mental effects of childbirth include:
1. Postpartum Anxiety (PPA)
Postpartum anxiety is a very common mental issue, with one out of five women experiencing it. There are several causes of postpartum anxiety, including:
- Hormonal changes- The sudden drop in progesterone and estrogen after birth might trigger anxiety.
- Lack of adequate support- New mothers need constant support and assurance, and lack of it causes anxiety.
- Previous mental health issues- Women who have previously been diagnosed with OCD, anxiety, and depression are at a higher risk of developing PPA.
- Thyroid imbalance- Postpartum thyroiditis causes the body to develop severe anxiety.
- Traumatic birth experience- Mothers who undergo emergency C-sections, birth complications, and NICU stays tend to develop constant fear and anxiety.
Symptoms of Postpartum Anxiety
There are emotional and physical symptoms of postpartum anxiety.
Emotional Symptoms
The emotional symptoms of postpartum anxiety include:
- Recurring, intrusive thoughts (e.g., “What if I drop the baby?”)
- Irrational fears (e.g., obsession over SIDS, germs, or harm coming to the baby)
- Overwhelming dread that something bad will happen
- Inability to relax even when the baby is safe/sleeping
- Guilt or shame about not being “good enough”
Physical symptoms of PPA
They include the following:
- Racing heart, dizziness, or panic attacks
- Stomachaches, nausea, or loss of appetite
- Muscle tension, headaches, or trembling
- Insomnia (even when the baby is asleep)
Management Tips for Postpartum Anxiety
These are the most effective management tips for PPA:
- Self-care strategies: Limiting caffeine and alcohol intake, eating healthy meals, and getting enough sleep.
- Professional help: Getting cognitive behavioral therapy (CBT), taking medication, and hormone testing.
- Emotional support: Talking to someone, writing down your thoughts, and challenging anxious thoughts.
2. Feeling Overstimulated
The overstimulation or feeling touched out experience is very common during pregnancy and postpartum. Several symptoms can easily tell that you are struggling with overstimulation:
- Irritability or anger when touched (even by loved ones).
- Crying or shutting down when overwhelmed.
- Feeling “claustrophobic” in your own body.
- Avoiding physical affection (even from your baby, which can trigger guilt).
- Constantly zoning out/dissociating to escape overstimulation.
3. Changes in Sex Drive and Vaginal Dryness
Changes in sex drive, such as low libido and vaginal dryness postpartum can be caused by the following:
Psychological factors
- Exhaustion due to insomnia and sleep deprivation.
- Body image concerns such as weight gain, postpartum saggy skin, or big breasts due to breastfeeding.

- Stress and anxiety linked to parenthood.
- Hormonal changes
- Lower estrogen levels when breastfeeding causes the vagina to become dry.
- An increase in prolactin (breastfeeding hormone) lowers estrogen and testosterone, hence low libido.
Vaginal dryness
- Low estrogen levels
- Lack of arousal due to a lack of enough foreplay
- High dehydration levels
Physical Recovery
- Vaginal soreness (from tearing, episiotomy, or C-section scar sensitivity).
- Pelvic floor weakness, which causes pain or incontinence during sex.
- Uterine contractions due to postpartum cramps, especially in early weeks.
Management Tips for Changes in Sex Drive and Vaginal Dryness

- Communicate with your partners about help with the baby, foreplay, mental and physical issues, etc.
- Seek hormonal help, like taking phytoestrogen-rich foods, Omega-3s & vitamin E, and birth control options.
- Emotional and mental recovery, such as adequate rest, couples therapy, and seeking self-pleasure first.
- Focus on outercourse (non-penetrative) intimacy first.
- Listen to your body’s response and only engage in intimacy when it is ready.
- Get pelvic floor therapy.
Final Thoughts
You just brought a new human being to the world. Congratulations. Now, go slow on yourself and let the body and mind heal. Don’t listen, read, or watch too much about how your favorite celebrity healed after delivering. Each person is unique, and so is motherhood.


